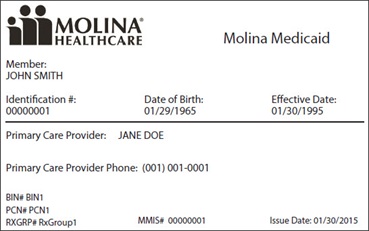
MEMBER INFORMATION Prescriber Name NPI Member Name Todays Date Prescriber Specialty Phone Member Plan ID Date of Birth Prescriber Address Drug Allergies. Showing Information For South Carolina Type Size.
 Molina Prior Authorization Form Fill Online Printable Fillable Dentist That Take Molina Insurance
Molina Prior Authorization Form Fill Online Printable Fillable Dentist That Take Molina Insurance
North Charleston SC 29423-0309.
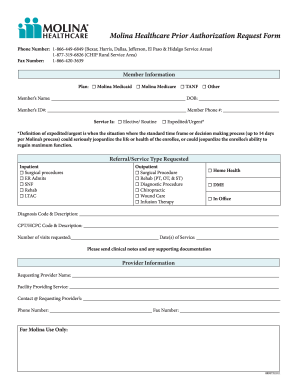
Molina healthcare of south carolina prior authorization form. Molina offers the following submission options. Medicaid Marketplace Medicare. 888 665-4621 PlanMedical Group Fax.
Select Health of South Carolina Subject. In order to request coverage for a patients prescription it may be necessary for the physician in question to submit a Molina Healthcare Prior Authorization Form. HospitalPrivate BH Practice Reference Guide.
Provider Dispute and Appeals. Prior Authorization Request Form. A few plans may continue to require prior authorization for mental health services.
It should be noted that the medical office will need to provide justification for requesting the specific medication and. Form Keywords prior autorization south carolina Medicaid SCDHHS Medicaid health plan prior auth drug medicine Created Date. To check the status of your request please call or visit our website.
Molina Healthcare of South Carolina. All fax requests will be processed in one business day. Find the Molina Healthcare Prior Authorization Request Form you require.
Nursing Facility Request Form. Submit Provider Disputes through the Contact Center at 855 882-3901. View the Molina Preferred Drug List.
Molina South Carolina Prior Authorization Form Author. Use one form per member please. Submit requests directly to Molina Healthcare of South Carolina via fax at 877 901-8182.
Hospice Services SCDHHSgov. Requirements established in South Carolinas State Plan the. US Legal Forms enables you to rapidly generate legally binding papers according to pre-built web-based templates.
MedicaidMyCare Authorization Form Community Behavioral Health. 01012021 FAX 866 423-3889 PHONE 855 237-6178. 2021 Behavioral Health Treatment Request Form Effective 010121 M EMBER I NFORMATION Line of Business.
Payment is made in accordance with a determination of the members eligibility benefit limitationexclusions evidence of medical necessity and other applicable standards during the claim review. Please fill out all applicable sections on both pages completely and legibly. Submit Provider Disputes through the Contact Center at 855 882-3901.
Molina Healthcare of Washington Prior Authorization Medication Exception Request Allow 2 business days to process Fax. Molina Healthcare Prior Authorization Request Form and Instructions. Provider Recovery Reversal Permission Form.
SOUTH CAROLINA MEDICAID PROGRAM. Chart notes or lab data to support the prior authorization request. ___ ___ _____ Fax completed forms to Magellan Rx Management.
Prior Authorization Service Request Form E FFECTIVE. Molina Healthcare of California PlanMedical Group Phone. Molina Healthcare of South Carolina uses a Preferred Drug List which lists the drugs that are covered by the health plan.
Attach any additional documentation that is important for the review eg. Prior Authorization PA Updates. HospitalPrivate BH Practice PA Form.
Perform your docs within a few minutes using our easy step-by-step guide. Prior Authorization Service Request Form E FFECTIVE. Although not eligible for managed care by virtue of dual.
Credentialing Checklist Practice Demographics Form Provider Change Form Primary Care Provider Change Request Form Contract Request Form October 2020 Provider Satisfaction Survey Claims Forms. Medicaid Marketplace Medicare. 01012021 FAX 866 423-3889 PHONE 855 237-6178 Molina Healthcare of South Carolina Inc.
The Act and 42 CFR 43151b prior authorization of or requiring the use. April 1 2021 I. Submit requests directly to Molina Healthcare of South Carolina via fax at 877 901-8182.
BH Prior Authorization Service Request Form FAX 866 423-3889 PHONE 855 237-6178 Molina Healthcare of South Carolina Inc. Universal Synagis Prior Authorization Form Provider NetworkCredentialing Forms. A Molina Healthcare Prior Prescription Rx Authorization Form can be used to request coverage for drugs that Molina Healthcare requires justification for prescribing.
Molina Healthcare of South Carolina Inc. South Carolina Medicaid Program General Prior Authorization Request Form Form must be complete correct and legible or the PA process can be delayed. Mental Health Prior Authorization.
2021 Prior Authorization GuideRequest Form Effective 010121. 2021 Prior Authorization GuideRequest Form medicaid carolina access prior authorization Verified 3 days ago. Submit requests via mail to.
- Prior Authorization Service. Submit requests directly to Molina Healthcare of South Carolina via the Provider Portal at. CBA is a separate company that administers mental health and substance abuse benefits on behalf of BlueCross BlueShield of South Carolina and BlueChoice HealthPlan.
Prior Authorization Code Matrix. Behavioral Health Respite Services PA Reference Guide. This list was carefully created by a group of pharmacists and physicians.
Contact Companion Benefits Alternatives CBA to verify by calling 800-868-1032. Molina Healthcare of South Carolina Inc. Medications Form must be complete correct and legible or the PA process can be delayed.